The somatosensory system is the anatomical and physiological neural substrate for detecting mechanical deformations of the skin, muscles, joints and other deep organs, conveying and processing that information through a number of pathways and neural centers, and eventually providing higher brain centers with the information needed to generate conscious perception of somatic sensations. Peripheral stimuli are transformed into neural impulses at the sensory receptors, and these impulses are conveyed through peripheral nerves to the dorsal horn of spinal cord and the dorsal column nuclei and trigeminal nuclei in the brain stem. The second processing station is the ventral posterior nuclear complex of the thalamus, from which the somesthetic information reaches the cerebral cortex. The whole system displays an exquisite spatial organization, which is reflected in a topologically continuous (somatotopic) arrangement of neuronal and axonal populations, with separate or intertwined "channels" specialized to convey and process different sensory submodalities. Representational "maps" arising from this anatomical and functional order, first described early in the XXth century, have been shown since the late 1970's to be anything but rigid and immutable, even in adult and aging individuals. Changes in these maps and in the underlying neural structures and circuits can be brought about by learning, experience, trauma, disease, or experimental manipulation of sensory input, sensory organs, nerves or centers, and are accompanied by a host of cytological changes that reflect alterations in gene expression and metabolic activities imposed by the altered input.
A practical adjunct of the knowledge derived from studying brain plasticity is a better understanding of the processes involved in the reaction of the neural structures to injury and disease, and the ability to design new therapeutic approaches applicable in the human and veterinary clinical settings. Agents and maneuvers intended to compensate for or repair structural and functional losses should take into account the possibilities, limits and characteristics of neural plasticity in normal and altered conditions, and their effects can now be assessed at molecular, anatomical, electrophysiological and behavioral levels. One such a reactive condition, which may result from disorders of the peripheral or central nervous system, is chronic pain, a cause of prime medical, social and economic concern in developed countries. Its treatment poses a greater challenge than acute pain, particularly when pain originates in nerve lesions, in what is known as neuropathic pain. Neuropathic pain syndromes of peripheral origin are common in clinical practice, and include painful conditions that accompany diabetes, cancer, and ischemia, post-amputation, post-deafferentation and phantom pain, and neuralgias of various kinds, in particular postherpetic and craniofacial.
Amongst the painful conditions in the craniofacial territory, apart from dental pain and temporomandibular disorders, migraine and painful trigeminal neuropathies are most prominent. These disorders are difficult to treat and their pathophysiology is harder to examine, because of the anatomical and functional complexities of the nerves and territories affected. Moreover, animal models developed for studying migraine and trigeminal pain are valuable, but limited, and this is partly responsible for the still incomplete knowledge of the pathophysiology of craniofacial pain conditions. Yet, four basic mechanisms involved in the generation and maintenance of chronic pain in general are likely to underlie this process also in the trigeminal territory: peripheral sensitization (due to changes in excitability of peripheral nerve fibers), central sensitization (due to an imbalance in neurotransmitters and receptors in the spinal cord and brain stem), reorganization of afferents, local neuronal circuits (in sensory ganglia, spinal cord and brain stem), and attenuation or loss of inhibitory mechanisms (in local circuits and descending modulatory connections). Microglia, the resident immune cells in the brain, are known to play significant roles in the latter three. An understanding of these mechanisms and processes is essential to define new therapeutic targets and assess the value of those currently used.
Specific research lines
Stability and mutability of ganglion cell populations in adult rats
Sensory input-dependent plasticity of specific cell populations of the mature trigeminal sensory system
Neural bases and mechanisms of chronic cephalic pain conditions
Techniques
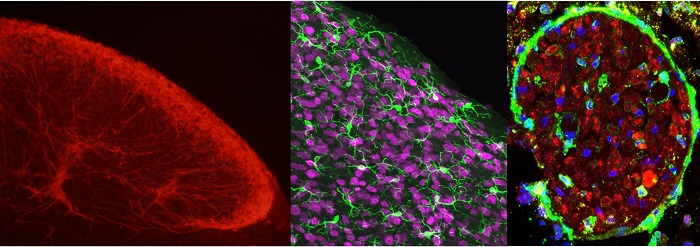
In vivo electrophysiological recordings -- Surgery of laboratory mammals -- Somatic sensory and motor behavioral testing of rodents -- Neuronal labeling using neural tracers and viral transduction -- Histology, Histochemistry and Immunohistochemistry -- Digital neuron reconstruction -- Confocal and electron microscopy -- Stereology
Lab Researchers
Lab Technician
Past Lab Members, current employment
Past Lab Members in training (15 years)
Degree / Current employment
Guadalupe Camarero Calderón
PhD / Guest Scientist, Charité, Berlin
Fivos Panetsos Petrova
PhD / Univ. Professor, Madrid
Bartolomé Bejarano Herruzo
PhD / MD, Neurosurgeon, Navarra.
Alfonso Lagares Gómez-Abascal
PhD / MD, Neurosurgeon & Professor, Madrid
Pilar Negredo Madrigal
PhD / Assoc. Professor, Madrid
Jorge Castro García
PhD / MSL Astra-Zeneca
José Antonio Villacorta
PhD / Assist. Professor, Madrid
Yasmina B. Martín Martínez
PhD / Assoc. Professor, Madrid
Silvia Pittolo
Master Deg / Postdoc, San Francisco, USA
Pedro E. Bermejo Velasco
PhD / MD, Neurologist, Madrid
Celia Herrera Rincón
PhD / Postdoc, Boston, USA
Laura Vázquez Martínez
Master Deg. / Research Techn., London
Julia Fernández Montoya
PhD / Research Assist., Cambridge, UK
Luke Diekhorst
Master Deg / PhD student, Madrid
Publications
- García-Magro Nuria, Martin Yasmina B., Palomino-Antolin Alejandra, Egea Javier, Negredo Pilar, Avendaño Carlos. 2019. Multiple Morphometric Assessment of Microglial Cells in Deafferented Spinal Trigeminal Nucleus. Frontiers in Neuroanatomy 13:103. doi: 10.3389/fnana.2019.00103
- García-Magro, N., Negredo, P., Martin, Y. B., Nuñez, Á., Avendaño, C. 2020. Modulation of mechanosensory vibrissal responses in the trigeminocervical complex by stimulation of the greater occipital nerve in a rat model of trigeminal neuropathic pain. The Journal of Headache and Pain, 21(1), 96. doi.org/10.1186/s10194-020-01161-y
- Garcia-Magro N, Martin YB, Negredo P, Avendano C. 2018. The greater occipital nerve and its spinal and brainstem afferent projections: A stereological and tract-tracing study in the rat. J Comp Neurol 26(18):3000-19. doi: 10.1002/cne.24511
- Fernández-Montoya J, Martin YB, Negredo P, Avendano C. 2018. Changes in the axon terminals of primary afferents from a single vibrissa in the rat trigeminal nuclei after active touch deprivation or exposure to an enriched environment. Brain Structure and Function, doi: 10.1007/s00429-017-1472-5:1-15.
- Perez-Laso C, Cerdan S, Junque C, Gomez A, Ortega E, Mora M, Avendano C, Gomez-Gil E, Del Cerro MCR, Guillamon A. 2018. Effects of Adult Female Rat Androgenization on Brain Morphology and Metabolomic Profile. Cereb Cortex 28(8):2846-53. doi: 10.1093/cercor/bhx163
- Fernandez-Montoya J, Avendano C, Negredo P. 2017. The Glutamatergic System in Primary Somatosensory Neurons and Its Involvement in Sensory Input-Dependent Plasticity. Int J Mol Sci 19. doi: 10.3390/ijms19010069
- Fernandez-Montoya J, Buendia I, Martin YB, Egea J, Negredo P, Avendano C. 2016. Sensory Input-Dependent Changes in Glutamatergic Neurotransmission- Related Genes and Proteins in the Adult Rat Trigeminal Ganglion. Front Mol Neurosci 9:132. eCollection@2016.:1-14.
- Parada E, Buendia I, Navarro E, Avendano C, Egea J, Lopez MG. 2015. Microglial HO-1 induction by curcumin provides antioxidant, antineuroinflammatory, and glioprotective effects. Mol Nutr Food Res 59:1690-700. doi: 10.1002/mnfr.201500279
- Martin, Y. B., Negredo, P., Villacorta-Atienza, J. A., and Avendano, C. Trigeminal intersubnuclear neurons: morphometry and input-dependent structural plasticity in adult rats.
J.Comp Neurol. 2014, 522:1597-1617. doi: 10.1002/cne.23494 - Parada E, Buendia I, Leon R, Negredo P, Romero A, Cuadrado A, Lopez MG, Egea J. 2014. Neuroprotective effect of melatonin against ischemia is partially mediated by alpha-7 nicotinic receptor modulation and HO-1 overexpression. J Pineal Res 56(2):204-12. doi: 10.1111/jpi.12113
- Parada E, Egea J, Buendia I, Negredo P, Cunha AC, Cardoso S, Soares MP, Lopez MG. 2013. The microglial alpha7-acetylcholine nicotinic receptor is a key element in promoting neuroprotection by inducing heme oxygenase-1 via nuclear factor erythroid-2-related factor 2. Antioxid Redox Signal 19(11):1135-48. doi: 10.1089/ars.2012.4671
- Herrera-Rincon C, Torets C, Sanchez-Jimenez A, Avendaño C, Panetsos F. Chronic electrical stimulation of transected peripheral nerves preserves anatomy and function in the primary somatosensory cortex. Eur J Neurosci. 2012 Dec;36(12):3679-3690. doi: 10.1111/ejn.12000
- Krzyzanowska A, Avendaño C. Behavioral testing in rodent models of orofacial neuropathic and inflammatory pain. Brain Behav. 2012 Sep;2(5):678-697. doi: 10.1002/brb3.85
- Krzyzanowska, A., Pittolo, S., Cabrerizo, M., Sanchez-Lopez, J., Krishnasamy, S., Venero, C., and Avendano, C. 2011. Assessing nociceptive sensitivity in mouse models of inflammatory and neuropathic trigeminal pain. J.Neurosci.Methods. doi:10.1016/j.jneumeth.2011.07.006
- Herrera-Rincon, C., Torets, C., Sanchez-Jimenez, A., Avendano, C., Guillen, P., and Panetsos, F. 2010. Structural preservation of deafferented cortex induced by electrical stimulation of a sensory peripheral nerve. Conf.Proc.IEEE Eng Med.Biol.Soc. 5066-5069. doi: 10.1109/IEMBS.2010.5626229
- Alfonso Lagares, Juan Jose Rivas, Luis Jiménez, Marta Cicuéndez, Carlos Avendaño. 2010. Central demyelination in the pathogenesis of trigeminal neuralgia associated with cerebellopontine angle tumors: case report with ultrastructural trigeminal root analysis. Neurosurgery 66:E841-E842. doi: 10.1227/01.NEU.0000367550.30165.A7 - selected as “Editor Choice” in the Journal: http://neurosurgerycns.wordpress.com/2010/04/15/.
- Yasmina B. Martin, Eduardo Malmierca, Carlos Avendaño, Angel Nuñez. 2010. Neuronal disinhibition in the trigeminal nucleus caudalis in a model of chronic neuropathic pain. Eur. J. Neurosci., 32:399-408. doi: 10.1111/j.1460-9568.2010.07302.x